
Goal
Improve pregnancy outcomes to maximize the lifelong health of women and their children.
Goal
Improve pregnancy outcomes to maximize the lifelong health of women and their children.

Research Opportunities
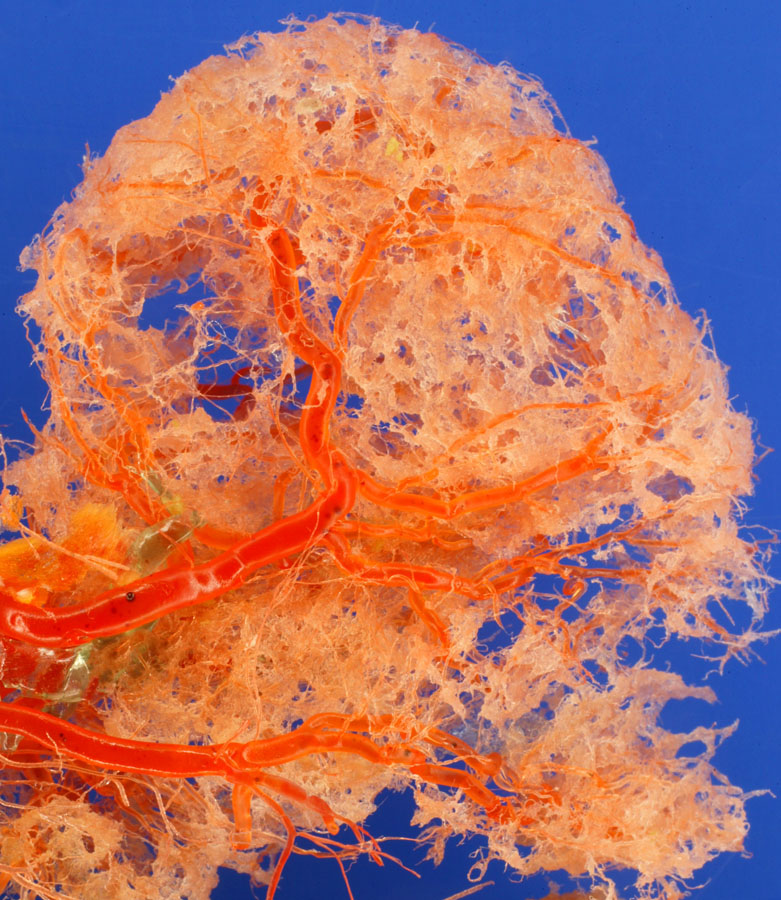
Exploring the developmental origins of health and disease is fundamental to the mission of NICHD. These efforts include the development of early indicators of threats to maternal health during pregnancy, such as preeclampsia, gestational diabetes, postpartum hemorrhage, and thromboembolism, to inform prevention efforts. This work also includes understanding how pregnancy-related conditions contribute to maternal morbidity and mortality, stillbirth, preterm birth, and the long-term health of women and their children. By studying the impact of genotypic, phenotypic, and environmental factors on pregnancy, researchers are now positioned to determine the biological underpinnings of complications and to identify potential targets for intervention. These efforts will incorporate new and/or existing datasets to better understand pre-pregnancy factors, such as obesity, and other conditions. Expanded study of the placenta, including noninvasive methods to determine placental health in real time, will play a key role in this research area. New prevention strategies will be discovered by considering maternal lifestyle factors (e.g., weight, exercise, and diet) and other influences before or during pregnancy that promote health or lead to disease. Using population health and other strategies, NICHD will strive to understand contributors to maternal morbidity and mortality, pregnancy loss, preterm birth, and neonatal morbidity and mortality. Understanding these factors will help to identify targets for effective prevention strategies and approaches to reducing health disparities. The evaluation of interventions early in pregnancy to protect the health of the woman and her fetus will be a vital component of this research.


Scientific Priorities to Advance Public Health
- Understand the human gestational clock and the potential causes of preterm birth through basic, translational, and clinical research.
- Improve the survival of infants born preterm or at low birthweight and optimize their outcomes by understanding the roles of early interventions, nutritional factors, the microbiome, and social and environmental support.
- Characterize pre-pregnancy and pregnancy factors that can raise the risk of adverse maternal conditions. Use emerging technologies and big data analytic methods, such as artificial intelligence, to integrate genomic, nutritional, social and behavioral, and exposure data to inform prevention efforts and address health disparities.
- Use basic and translational science approaches to further elucidate the role of the placenta in pregnancy outcomes and in the long-term health of the mother and infant. Continue to develop technologies and methods to monitor the placental function of animal models and humans in real time.
- Develop targeted strategies to improve the prevention of and response to labor and delivery complications that lead to maternal morbidity and mortality. Extend studies of key adverse events to the postpartum period (“the fourth trimester”) to include hemorrhage, mental health conditions, and cardiovascular events, emphasizing populations affected by health disparities.
 BACK TO TOP
BACK TO TOP